Biomag - Encyclopedia - Leg ulcer
Leg ulcer - symptoms, description and treatment
Revision

Does a small scratch or abrasion turn into a swollen, hard-to-heal wound? Or does a scab form that cracks and the wound becomes infected? It may be a leg ulcer, venous ulcer, ulcus cruris in Latin. These are painful and difficult to treat wounds that can have a serious impact on your daily life. The resulting wound often serves as a gateway for infections. The disease often affects people with reduced vascular blood flow, diabetics.
Find out what are the treatment options for leg ulcers. How to suppress symptoms such as pain, inflammation and poor blood circulation that accompany this disease? Read more here.
Leg ulcers symptoms
- Painful wound on the shin or in the foot area
- Itchiness
- Swelling
- Change in skin colour on the extremity
- Feeling of heavy legs
- Signs of infection (fever, weakness)
- Unpleasant smelling fluid coming from the wound [1]

Only a doctor can make a correct diagnosis. Do not use this or any other article on the internet to make a diagnosis. Don’t put off seeing a doctor and address your condition early.
Description and causes of leg ulcer

Definition of leg ulcers
What is a leg ulcer? It is a long-term disruption of tissue and the formation of a wound in the area of the tibia. The tibia is the part of the leg between the ankle and the knee. It consists of the calf (back of the leg) and the shin (front of the leg). However, ulcers can also occur between the toes or on the toes. [2][3]
A leg ulcer can vary in size, shape, colour and other characteristics. The exact form and mode of occurrence depends on what is the cause of the leg ulcer.
Some patients may be able to recognize the onset of aleg ulcer by swelling of the lower extremities, darkening of the skin, and thinning of the skin. The skin is then more susceptible to injury and subsequent ulceration. [4]
Do not underestimate the first symptoms. If you suspect that a leg ulcer is starting, see a doctor in its early stages.
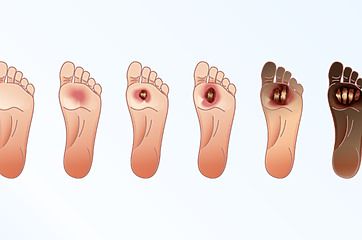
Venous ulcers photo gallery
Leg ulcer - causes
The primary cause of leg ulcer is vascular disease. Leg ulcers are not a disease in themselves, but a symptom of some other disease.
- 73% of legulcers are venous in origin. Professionally, venous ulcers are called ulcus cruris venosum.
- 8% of ulcers are related to artery disease. Doctors talk about an arterial ulcer – ulcus cruris arteriosum.
- 3% of leg ulcers are caused by diabetes.
- 2% of ulcers occur after trauma.
- 14% of ulcers have other causes. If there are several causes at the same time, it is ulcus cruris mixtum.[5]
Types of leg ulcers and their description
- Leg ulcers of venous origin
It is caused by the accumulation of venous blood in the legs. It is a complication of chronic venous insufficiency. [6 ] Risk factors include a history of inflammation in the deep venous system, hereditary predisposition to venous disease, obesity, lack of exercise and sedentary occupation[7].
What do venous ulcers look like? They are usually smaller, shallow and have smooth edges. They are less painful than other types of leg ulcers. If patients report pain, it is usually related to the onset of inflammation. [8] - Leg ulcer of arterial origin
Arterial ulcers arise due to diseases of the arteries that affect the lower limbs. The main problem is the narrowing of the arteries. They occur more often in the elderly and in patients with high blood pressure.
What do arterial ulcers look like? They are most commonly found on the heel, on the toes and around the ankle. Compared to other ulcers, they are deeper and have pronounced margins. Typical is great soreness, which intensifies at night when the legs are laid flat on the bed.[9] - Diabetic leg ulcer
It is associated not only with diseases of the arteries and nerves on the peripheral parts of the body, but also with high blood sugar.[10]
What do leg ulcers look like in diabetes? They appear on the toes, on the soles of the feet and on the shins. The ulcers are not large, but they are deep and can extend to the bone. There is hardened skin around the ulcer.[11] More on the diabetic foot diagnosis page. - Other types of leg ulcers
Leg ulcers can also be related to a number of other diseases. They occur, for example, in patients with rheumatoid arthritis (an autoimmune disease affecting the joints), in some cancers or in intestinal inflammation.[12]
Risk factors for leg ulcer
Seniors areat risk of developing leg ulcers, especially if they have diabetes, high blood pressure and are overweight. [13]
The risk also increases:
- deep vein thrombosis (a blood clot that clogs a vein),
- varicose veins on the legs,
- a previous fracture, injury or surgery to the leg that restricts walking and impairs blood flow.[14]
Diagnostics - how to recognize leg ulcers?
If you suspect a leg ulcer, see a doctor as soon as possible. Without proper treatment, leg ulcers will not heal on their own. The doctor must determine the cause of their occurrence, otherwise the risk of worsening the condition or recurrence of ulcers increases.[15]
How is the examination of leg ulcers carried out?
The first step is to find out information – so expect questions about the start of the problem, your general health and your employment. The doctor will then examine you carefully and determine further tests accordingly.
- The condition of the feet, location, size, shape and characteristics of the ulcers are determined by inspection. The doctor also monitors the possible appearance of varicose veins, swelling and skin color. All this is done standing and lying down.
- By palpation, the doctor assesses the temperature and tension of the skin, swelling and the characteristics of the ulcer itself.
- During the blood draw, blood count, blood sugar and other values are checked.
- In some cases, a tissue sample is taken from the leg ulcer for microbiological examination. [16]
Doppler test

The Doppler test is an ultrasound examination of the blood vessels in the legs. In addition to displaying blood vessels, it can measure blood flow velocity. Thanks to this painless examination, the doctor gets an overview of the possible vascular causes of leg ulcers.
The examination is usually accompanied by a check of blood pressure in the ankle area to assess the ankle index.[17]
Did you know?
- Up to 5% of people over the age of 70 suffer fromleg ulcers.
- The majority (80%) of ulcers are caused by vascular insufficiency.
- The most common complication of leg ulcers is infection. [18]
Complications when left untreated
If a leg ulcer is not treated or the treatment is not effective, complications can occur with a significant impact on your life.
- Infection: an open wound resulting from a leg ulcers ulcer is a gateway for infection.
- Chronic pain: untreated can lead to permanent pain and limitations in daily life.
- Swelling and fever: Harmful microorganisms enter through an open wound and cause redness, swelling and fever.
- Rosacea: It is a bacterial infection of the skin.
Infection
Chronic pain
Swelling and fever
Rosacea

We recommend not postponing treatment of leg ulcers
Do not delay treatment for a leg ulcers and see a specialist if you have any health problems or doubts about your health. This will prevent unnecessary health complications.
Treatment of leg ulcers
Treatment of leg ulcers is carried out in several ways. Doctors from different disciplines work together.
Local treatment involves taking care of the ulcer itself, which must be cleaned and then treated with special preparations so that the wound can heal successfully. Dead tissue impedes healing, which is why its removal is so important.
The wound then requires the maintenance of a reasonably moist environment. This is helped by a number of modern means for so-called moist healing. [19]
Compression therapy belongs to the standard treatment of leg ulcers. It uses compression (tightening) elastic stockings or a bandage. The aim is to promote the proper functioning of the blood circulation.[20] The decision whether to use stockings or bandages depends on the stage of the disease, the condition of the lower limbs and the patient’s cooperation. In general, elastic bandages are used in the acute phase and tightening stockings in long-term treatment. Compression therapy is not used, for example, in patients with severe heart problems. [21]
The overall treatment of leg ulcers depends on what is causing them. Various drugs are used to treat vascular diseases, which counteract swelling, promote blood flow and have an anti-inflammatory effect. Patients also take medication for other conditions (such as diabetes). Pain killers are also sometimes needed and antibiotics in case of infection. [22][23]
Invasive treatment (surgery) comes into play when there is a need to improve blood circulation to the leg and to treat non-healing leg ulcers with vascular surgery. [24] Surgery for leg ulcers is performed at a specialised vascular surgery unit where different types of surgery are performed.

Beware
The treatment of leg ulcers can only be determined by your doctor after considering your overall health. Therefore, do not use this article as a guide to treatment, which can only be determined by a doctor.
Moist wound healing - also helps with leg ulcers

There is a wide range of products that are used in wound care and also help in the treatment of leg ulcers. You should therefore leave the choice of the appropriate cover for ulcers to your doctor.
Various gels, dressings called hydrocolloids, seaweed coverings or special dressings that absorb secretions (fluid) from the legulcer are used for treatment. A covering containing silver also helps in the treatment of chronic wounds. [25]
Home treatment of leg ulcers - home remedies
In home care for leg ulcer, various regimen measures and herbal products are used.
- Treat your body with substances called bioflavonoids. They are contained in, for example, blueberries, parsley, horseradish and red cabbage.
- Include rosehip tea in your drinking regime.
- Make sure your feet are warm and wear socks that don’t pinch. Both are important for maintaining good blood circulation. Poor blood circulation creates conditions for the development of leg ulcers.
- Poultices for leg ulcers can be prepared from horsetail or horsetail root. [26]
What to apply to leg ulcers? You can try ointment from calendula or marigold. These are herbs with healing effects.
Before you reach for herbs, whether in the form of teas or directly for wound care, consult your doctor. Caution is needed when using herbs, especially if you are taking medication.
However, grandmotherly advice for leg ulcers may not be effective as a full-fledged modern treatment, we always recommend visiting a specialist and discussing the treatment with him.
Prevention of leg ulcers
The best cure for legulcers is prevention. The following steps are important for her. They mainly concern at-risk groups and people who have had a history of leg ulcers.
- Follow the prescribed treatment for diseases that can cause leg ulcers (for example, diabetes or high blood pressure).
- Try to lose weight if you are overweight.
- Stop smoking cigarettes.
- Regularly engage in physical activities.
- Take care of your feet – prop them up when you sit at work and regularly give them a raised position at home.
- Ask your doctor how often to wear tightening stockings. [27][28]
Leg ulcers and baths
Ask your doctor about spa treatment options for leg ulcers. It will tell you all the latest information and specific recommendations. Various special methods of ulcer care are used in the spa – for example, light therapy or electromagnets (magnetic therapy). [29][30]

Important information when dealing with leg ulcers
Typhoid ulcers require medical attention.
Take care of your feet.
Move regularly – you promote blood circulation.
When treating leg ulcers, do not automatically “demand” antibiotics.
Summary and recommendations for the management of leg ulcers
See a doctor
The treatment of a leg ulcer is always determined by a doctor based on a general examination, an assessment of your health and an accurate diagnosis.
Causal treatment of leg ulcers
After a general examination, your doctor will recommend treatment for the cause of the leg ulcer. They will also advise you on possible lifestyle adjustments and the next course of action.
Relieving pain, improving blood circulation and resolving inflammation
Symptomatic treatment focuses on the symptoms of the disease. Such treatment can significantly improve your quality of life and support comprehensive treatment during the course of the disease.
Sources, references and literature
[1] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[2] Stryja J. Treatment of infected tibial ulcer. Dermatol. Practice 2021; 15(4): 191-194. https://www.solen.cz/pdfs/der/2021/04/03.pdf
[3] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[4] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[5] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[6] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[7] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[8] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[9] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[10] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[11] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[12] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[13] Leg ulcers. Healthdirect Australia, April 2021. https://www.healthdirect.gov.au/leg-ulcers
[14] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[15] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[16] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[17] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[18] Stryja J. Treatment of infected tibial ulcer. Dermatol. Practice 2021; 15(4): 191-194. https://www.solen.cz/pdfs/der/2021/04/03.pdf
[19] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[20] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[21] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[22] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[23] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[24] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[25] Karen I., Švestková S. Chronic ulcer of the lower limb. Recommended diagnostic and therapeutic procedure for general practitioners. Society of General Medicine ČLS, Prague 2007. https://www.svl.cz/files/files/Doporucene-postupy-2003-2007/Vred-DK.pdf
[26] Mlčoch Z. Tongue ulcers – herbs, herbs, herbal advice, poultices, ointments, treatment, recommendations and measures. Herbs for all, 19. March 2015. https://www.bylinkyprovsechny.cz/nemoci/ruzne-nemoci/783-bercove-vredy-byliny-bylinky-babske-rady-obklady-masti-lecba-doporuceni-a-opatreni
[27] Venous leg ulcer. NHS, 16. November 2022. https://www.nhs.uk/conditions/leg-ulcer/
[28] Leg ulcers. Healthdirect Australia, April 2021. https://www.healthdirect.gov.au/leg-ulcers
[29] Electrotherapy. Spa hotel Prusik, Konstantinovy Lazne. https://www.konstantinovylazne.cz/cz/lecba/lecebne-procedury/elektrolecba/
[30] Magnetotherapy treatment. Karlova Studénka Mountain Spa. https://www.horskelazne.cz/bazen-a-procedury/procedury/magnetoterapie
| Rate this article |
|
|
5/51 Reviewed by
|
How to control pain, swelling, inflammation and promote healing?
The solution may be symptomatic treatment using pulsed magnetic therapy, which targets signs and symptoms such as pain, swelling and reduced blood flow. In addition, such treatment can support comprehensive treatment and significantly improve quality of life.
Explaining the effects
The basic principle of Biomag 3D pulsed magnetic therapy (PEMF)is the generation of electromagnetic pulses. These pulses penetrate through the clothing and through the entire depth of the tissue to the point of targeted application. The pulses have specially developed biotropic parameters (e.g. frequency, shape, intensity) to best affect various health problems.
What are the effects of 3D magnetic therapy (PEMF therapy)?
- It helps to relieve pain.
- Anti-inflammatory.
- Promotes blood circulation.
How is the therapy applied?
The application is very simple. Select the desired therapeutic effect on the device and attach the connected applicator to the desired application site. Magnetic therapy is usually applied 2 times a day for 20 minutes.
We will be happy to help you try this method and advise you on which device to purchase.